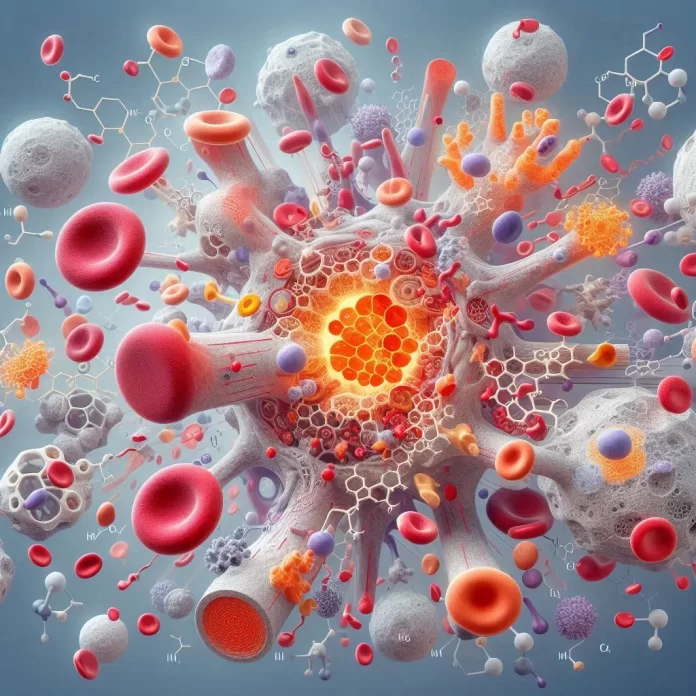
Blood coagulation is a complex yet vital process that prevents excessive bleeding and promotes wound healing following an injury. Central to this process is calcium, a key element that mediates several critical steps within the coagulation cascade. From platelet activation to thrombin formation and the activation of Factor XIII, calcium ensures the efficient and timely formation of stable blood clots. This article explores the multifaceted roles of calcium in these processes, shedding light on the mechanisms involved and the potential therapeutic implications for treating various coagulation disorders.
I. Understanding Platelet Activation by Calcium:
Platelet activation is a crucial process in the body’s response to injury, leading to blood clotting and wound healing. Calcium plays a central role in this activation, mediating various biochemical pathways that ensure efficient platelet function.
1. The Role of Calcium in Platelet Activation:
When an injury occurs, platelets are one of the first responders to the site. The activation of platelets is heavily dependent on the rise in intracellular calcium levels. This increase in calcium concentration is facilitated by two primary mechanisms:
– Release from Intracellular Stores:
Platelets contain internal reservoirs of calcium, known as the dense tubular system (DTS). Upon activation, calcium is released from these stores into the cytoplasm.
– Calcium Entry from Extracellular Space:
Platelets also have various calcium channels on their surface that open to allow calcium influx from the surrounding blood plasma.
-This dual mechanism ensures a rapid and sufficient rise in cytosolic calcium, which is essential for platelet activation.
2. Mechanisms of Platelet Activation:
The increase in cytosolic calcium concentration triggers several downstream events critical for platelet activation:
– Shape Change:
Platelets undergo a transformation from a discoid shape to a more spherical form with extended filopodia, which aids in their adhesion to the injury site.
– Granule Secretion:
Activated platelets release granules containing various substances such as ADP, thromboxane A2, and serotonin, which amplify the activation signal and recruit more platelets to the site.
– Surface Receptor Activation:
Calcium signaling leads to the activation of integrins and other surface receptors on platelets, enhancing their ability to stick to the damaged blood vessel walls and each other, forming a platelet plug.
-These processes collectively contribute to the formation of a stable blood clot, which is essential for stopping bleeding and initiating wound healing.
3. Benefits of Platelet Activation:
The activation of platelets through calcium signaling has several key benefits:
– Hemostasis:
The primary benefit is the cessation of bleeding. By forming a platelet plug, the body prevents excessive blood loss and protects the integrity of the circulatory system.
– Wound Healing:
Platelets release growth factors and other bioactive molecules that promote tissue repair and regeneration at the injury site. These factors stimulate the proliferation and migration of cells necessary for wound healing.
– Immune Response:
Platelets play a role in the immune response by interacting with leukocytes and releasing antimicrobial peptides, which help protect against infection at the injury site.
4. Therapeutic Implications:
Understanding the role of calcium in platelet activation also has important therapeutic implications. For instance, in conditions where excessive platelet activation leads to thrombosis (such as in heart attacks or strokes), targeting calcium signaling pathways can help develop drugs that inhibit platelet activation and prevent unwanted clot formation.
5. Implications and Future Prospects of Calcium-Induced Platelet Activation:
Calcium’s role in platelet activation is a finely tuned process essential<span data-preserver-spaces=”true”> for effective hemostasis and wound healing. The benefits of this activation extend beyond merely stopping bleeding, playing a crucial role in tissue repair and immune defense. Advances in understanding these mechanisms open up potential therapeutic avenues for treating various thrombotic disorders.
II. Understanding Thrombin Formation Through Calcium:
The formation of thrombin is a critical step in the blood coagulation process, essential for stopping bleeding and initiating wound healing. Calcium plays a pivotal role in this process by facilitating the conversion of prothrombin to thrombin.
1. Role of Calcium in Thrombin Formation:
Thrombin formation is a multi-step process within the coagulation cascade, where calcium ions are crucial at several stages:
– Activation of Factor X:
Calcium ions are necessary for the activation of Factor X to Factor Xa. This activation is a key step as Factor Xa combines with Factor V to form the prothrombinase complex, which catalyzes the conversion of prothrombin to thrombin.
– Prothrombinase Complex Formation:
Calcium ions facilitate the binding of prothrombin to the prothrombinase complex on the surface of activated platelets. This binding is essential for the efficient conversion of prothrombin to thrombin.
-Without sufficient calcium levels, the formation of thrombin would be inefficient, leading to impaired blood clotting and potential excessive bleeding.
2. Mechanisms of Thrombin Formation:
The conversion of prothrombin to thrombin involves several critical steps:
– Binding to Phospholipids:
Calcium ions enable the binding of prothrombin to negatively charged phospholipids on the surface of activated platelets. This positioning is crucial for the subsequent enzymatic reactions.
– Cleavage by Prothrombinase:
The prothrombinase complex, facilitated by calcium, cleaves prothrombin at specific sites, producing active thrombin. This reaction is highly regulated and occurs rapidly to ensure efficient clot formation.
-The generated thrombin then plays a central role in converting fibrinogen to fibrin, forming the structural basis of a blood clot.
3. Benefits of Thrombin Formation:
The formation of thrombin via calcium-dependent pathways provides several vital benefits:
– Hemostasis:
Thrombin is essential for converting soluble fibrinogen into insoluble fibrin, which forms the meshwork of a blood clot. This process is critical for stopping bleeding and preventing excessive blood loss.
– Activation of Coagulation Factors:
Thrombin activates several other coagulation factors (e.g., Factors V, VIII, XI, and XIII), amplifying the coagulation cascade and ensuring robust clot formation.
– Wound Healing:
Thrombin promotes tissue repair by stimulating the release of growth factors from platelets and endothelial cells, which aid in wound healing and tissue regeneration.
4. Therapeutic Implications:
Understanding the role of calcium in thrombin formation has significant therapeutic implications. For instance, in conditions where thrombin formation is excessive, such as in certain thrombotic disorders, targeting calcium-dependent steps can help develop anticoagulant therapies. Conversely, in cases of bleeding disorders, ensuring adequate calcium levels can support proper coagulation and clot formation.
5. Implications and Future Prospects of Calcium-Dependent Thrombin Formation:
Calcium’s role in thrombin formation is a finely regulated process essential<span data-preserver-spaces=”true”> for effective hemostasis and wound healing. The benefits of this process extend beyond merely stopping bleeding, playing a crucial role in activating other coagulation factors and promoting tissue repair. Advances in understanding these mechanisms open up potential therapeutic avenues for treating various coagulation disorders and improving clinical outcomes in patients with bleeding or thrombotic conditions.
III. The Role of Calcium in Factor XIII Activation:
Calcium is a crucial element in activating Factor XIII, an important enzyme in blood coagulation. This article delves into how calcium facilitates the activation of Factor XIII and the benefits of this process in wound healing and maintaining hemostasis.
1. Role of Calcium in Factor XIII Activation:
Factor XIII, also known as the fibrin-stabilizing factor, plays a vital role in the final stages of blood coagulation. The activation process involves several key steps:
– Thrombin Cleavage:
Thrombin activates Factor XIII by cleaving its activation peptide. This reaction is calcium-dependent, as calcium ions are necessary for the structural changes that allow thrombin to access and cleave Factor XIII.
– Formation of Factor Xia:
Once cleaved by thrombin, Factor XIII becomes Factor XIIIa, an active enzyme that cross-links fibrin, stabilizing the clot.
This activation is essential for the proper function of Factor XIII, ensuring that clots are stable and durable.
2. Mechanisms of Factor XIII Activation:
The activation of Factor XIII by calcium involves:
– Binding to Fibrin:
Calcium ions facilitate the binding of Factor XIII to fibrin, positioning it correctly for activation by thrombin.
– Structural Changes:
Calcium induces conformational changes in Factor XIII, exposing the activation sites for thrombin. This process ensures efficient activation and the formation of a stable clot.
3. Benefits of Factor XIII Activation:
The activation of Factor XIII provides several critical benefits:
– Clot Stabilization:
Factor XIIIa cross-links fibrin strands, making the blood clot more resistant to mechanical stress and fibrinolysis (the breakdown of clots). This stabilization is crucial for maintaining hemostasis, especially in areas subject to movement or pressure.
– Wound Healing:
By stabilizing clots, Factor XIIIa provides a scaffold for tissue repair. It also plays a role in angiogenesis (the formation of new blood vessels) and the overall healing process by supporting the formation of a stable environment for new tissue growth.
– Reduced Bleeding:
Stable clots prevent re-bleeding, which is especially important in conditions like surgery or trauma. Proper activation of Factor XIII ensures that clots remain intact until the wound is fully healed.
4. Therapeutic Implications:
Understanding the role of calcium in Factor XIII activation has significant therapeutic implications. For individuals with Factor XIII deficiency or dysfunctional calcium signaling, therapies to enhance this pathway could improve clot stability and wound healing. Conversely, in conditions where excessive clot stability is problematic, such as in certain thrombotic disorders, targeting calcium-dependent activation steps might provide new treatment strategies.
5. Implications and Future Prospects of Calcium-Dependent Factor XIII Activation:
Calcium’s role in the activation of Factor XIII is critical for effective blood clot stabilization and wound healing. This process ensures that clots are robust and resistant to premature breakdown, which is essential for maintaining hemostasis. Advances in understanding these mechanisms offer potential therapeutic avenues for improving clinical outcomes in patients with coagulation disorders or those undergoing surgical procedures.
IV. Understanding the Coagulation Cascade: The Role of Calcium in Injury Response.
The coagulation cascade is a complex sequence of events crucial for stopping bleeding and initiating wound healing. Calcium plays a pivotal role in this cascade, enabling the activation of various clotting factors.
1. Role of Calcium in the Coagulation Cascade:
Calcium ions are essential at multiple steps in the coagulation cascade. They act as cofactors, facilitating the activation of key clotting factors:
– Activation of Factor X:
One of the central steps in the coagulation cascade is the activation of Factor X to Factor Xa. Calcium ions bind to Factor X, along with other cofactors, forming a complex essential for its activation. This step is crucial as Factor Xa converts prothrombin to thrombin.
– Conversion of Prothrombin to Thrombin:
Thrombin is a vital enzyme that converts fibrinogen to fibrin, forming the mesh-like structure that stabilizes the blood clot.
Calcium ions are necessary for the proper functioning of thrombin, ensuring efficient clot formation.
– Activation of Factor XIII:
Once fibrin is formed, Factor XIII, also dependent on calcium, cross-links the fibrin strands, making the clot more stable and resistant to breakdown. This step is crucial for the integrity and durability of the blood clot.
2. Mechanisms of Calcium in the Coagulation Cascade:
The coagulation cascade involves a series of tightly regulated steps:
– Intrinsic and Extrinsic Pathways:
The coagulation cascade is initiated via two primary pathways—intrinsic and extrinsic. Both pathways converge on the activation of Factor X. Calcium ions are required at multiple points within these pathways to facilitate the interactions between various clotting factors and their activation.
– Common Pathway:
Once Factor X is activated, it enters the common pathway, leading to the conversion of prothrombin to thrombin and the subsequent formation of a fibrin clot. Calcium ions are integral in stabilizing these reactions and ensuring they occur efficiently.
3. Benefits of Calcium-Dependent Coagulation:
The activation of the coagulation cascade by calcium ions provides several critical benefits:
– Hemostasis:
The primary benefit is the prevention of excessive blood loss. By facilitating the rapid formation of a stable clot, calcium ensures that bleeding is quickly controlled at the site of injury.
– Wound Healing:
The formation of a stable fibrin clot creates a scaffold for tissue repair and regeneration, promoting faster wound healing and reducing the risk of infection.
– Prevention of Re-bleeding:
Calcium-dependent stabilization of the blood clot ensures that it remains intact until the underlying tissue has sufficiently healed, preventing re-bleeding and ensuring effective hemostasis.
4. Therapeutic Implications:
Understanding the role of calcium in the coagulation cascade has significant therapeutic implications:
– Bleeding Disorders:
For individuals with deficiencies in calcium or clotting factors, therapies aimed at enhancing calcium availability or mimicking its action could improve coagulation and reduce bleeding risks.
– Anticoagulant Therapy:
In conditions where excessive clotting is a concern, such as in thrombotic disorders, targeting calcium-dependent steps in the coagulation cascade can help develop anticoagulant therapies that prevent inappropriate clot formation.
5. Implications and Future Prospects of Calcium-Dependent Coagulation:
Calcium’s role in the coagulation cascade is vital for maintaining hemostasis and ensuring effective wound healing. By facilitating the activation of key clotting factors, calcium ensures that blood clots form rapidly and are stable. Advances in understanding these mechanisms can lead to improved treatments for bleeding disorders and the development of targeted anticoagulant therapies, enhancing clinical outcomes for patients with coagulation-related conditions.
Conclusion:
Calcium is indispensable in the intricate processes of blood coagulation, playing pivotal roles in platelet activation, thrombin formation, and the stabilization of blood clots through Factor XIII activation. These calcium-dependent pathways are essential not only for preventing excessive bleeding and ensuring effective hemostasis but also for promoting tissue repair and immune defense. Understanding these mechanisms provides valuable insights into developing targeted therapies for both bleeding and thrombotic disorders, paving the way for improved clinical outcomes and enhanced patient care in the realm of coagulation-related conditions.