Kidney stones, those painful crystalline formations within the renal system, can significantly disrupt a person’s health and quality of life. While factors contributing to their formation are varied, one lesser-known but crucial element is dietary salt intake. This article delves into the intricate relationship between salt consumption and kidney stone development, exploring the physiological mechanisms and the impactful role of dietary choices. Understanding this connection is essential not only for those currently suffering from kidney stones but also for anyone looking to prevent their occurrence through proactive dietary management.
I. Understanding Kidney Stones: Types and Composition.
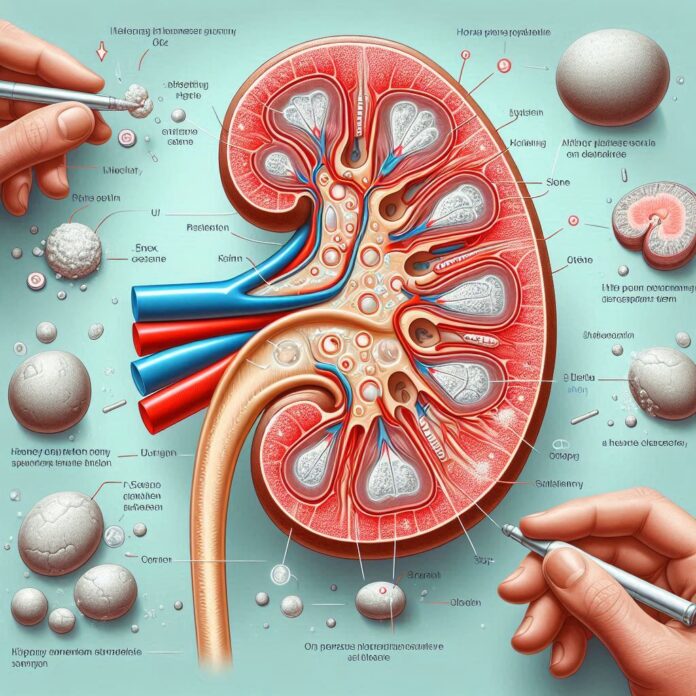
Kidney stones, or renal calculi, are solid masses made of crystals. They typically originate in your kidneys but can develop anywhere along your urinary tract, which includes the kidneys, ureters, bladder, and urethra. Understanding the different types of kidney stones and their compositions is crucial for both medical professionals and patients to manage and prevent these painful conditions effectively.
1. Types of Kidney Stones:
Kidney stones vary significantly in chemical composition, each type having specific causes and treatments:
-Calcium Stones:
•Calcium Oxalate: The most common type of kidney stone, forms when calcium combines with oxalate in the urine. Increased levels of calcium or oxalate can occur due to food, high doses of vitamin D, intestinal bypass surgery, and several metabolic disorders.
•Calcium Phosphate: Less common than calcium oxalate stones, calcium phosphate stones occur in alkaline urine. They can be associated with certain metabolic conditions, such as renal tubular acidosis, and can sometimes occur in those who take medications to prevent migraines or seizures.
-Uric Acid Stones:
•Formed when the urine is consistently acidic. A diet rich in purines substances found in animal protein such as meats, fish, and shellfish can increase uric acid in urine. Uric acid stones are more common in men than in women and can also occur with gout or chemotherapy.
-Struvite Stones:
These stones form in response to an infection, such as a urinary tract infection. They can grow quickly and become quite large, sometimes with few symptoms or little warning.
-Cystine Stones:
These stones form in people with a hereditary disorder called cystinuria which causes the kidneys to excrete too much of a specific amino acid (cystine). Cystine can build up in the urine to form crystals and stones.
2. Composition and Structure:
The composition of kidney stones is a key factor in determining the most effective treatment plan and preventive measures:
-Calcium Oxalate:
Rough and jagged, these stones are often difficult to pass and can be painful. They are often managed through diet, hydration, and in some cases, medications that reduce calcium or oxalate levels.
-Calcium Phosphate:
These stones are typically smoother than oxalate stones and often form in people with metabolic conditions that raise the pH of the urine.
-Uric Acid Stones:
These stones are softer and smoother than calcium stones. Treatment may include medications that alkalinize the urine, such as potassium citrate, as well as reducing intake of purine-rich foods.
-Struvite Stones:
These stones are often larger with a staghorn appearance that can occupy a large portion of the kidney. Treatment often involves eradicating the underlying infection with antibiotics and sometimes requires surgical removal of the stone.
-Cystine Stones:
Often recurring and resistant to treatment, these stones might need lifelong medication to control and significant lifestyle and dietary changes to manage cystine levels.
3. Diagnostic and Management Strategies for Different Stone Types:
Understanding the types and compositions of kidney stones not only aids in appropriate treatment but also helps in the implementation of dietary and lifestyle changes necessary to prevent their recurrence. Each type of stone has specific triggers and treatment strategies, making it essential to identify the stone type through diagnostic testing.
II. Salt Intake and Its Role in Stone Formation:
The connection between salt intake and kidney stone formation involves several physiological mechanisms:
1. Increased calcium excretion:
High salt consumption leads to greater sodium presence in the kidneys, which promotes calcium excretion in urine. This excess calcium can precipitate with oxalate or phosphate, forming stones.
2. Dehydration and urine concentration:
Excess salt can cause dehydration, as the body uses more water to flush out sodium. Concentrated urine then becomes a more conducive environment for stone formation due to higher levels of dissolved minerals.
3. Changes in urine pH:
Different types of salts can alter urine pH, affecting stone risk. For example, sodium increases urine pH, enhancing the risk of calcium stones, while potassium-containing salts may reduce pH, increasing the risk of uric acid stones.
4. Reduced citrate excretion:
Sodium can interfere with the reabsorption of citrate, a molecule that helps prevent stone formation by binding with urinary calcium. Lower citrate levels in the urine thus promote stone formation.
5. Impact on oxalate levels:
High salt intake can also affect the intestinal handling of oxalate, a key component in calcium oxalate stones. More oxalate may be absorbed into the bloodstream and subsequently excreted in the urine, increasing stone risk.
III. Preventive Measures and Dietary Recommendations:
Managing salt intake and adopting specific dietary strategies can significantly reduce the risk of kidney stone formation. This section delves deeper into the recommended preventive measures and dietary changes that can help avoid the development of kidney stones.
1. Lower Sodium Intake:
-Target Levels:
It’s advisable to limit sodium intake to less than 2,300 mg per day, which aligns with the guidelines provided by health organizations like the American Heart Association.
-Practical Tips:
Avoid processed foods, which often contain high levels of sodium. Opt for fresh or frozen produce, and season dishes with herbs and spices instead of salt. Reading food labels diligently to check sodium content can also help manage intake.
2. Increase Water Consumption:
-Hydration Goals:
Aim to drink at least 2 to 3 liters of water daily. This helps to dilute the urine, reducing the concentration of minerals that can form stones.
-Benefits:
Proper hydration not only prevents the formation of new stones but also aids in the passage of small stones and crystal fragments.
3. Balanced Calcium and Oxalate Intake:
-Calcium Intake:
Ensure a daily intake of calcium appropriate for your age and health needs, which can help reduce oxalate levels in the urine by binding with oxalate in the gut.
-Oxalate Management:
Limit intake of oxalate-rich foods such as spinach, rhubarb, and almonds, especially in individuals with a history of oxalate stones. Combining oxalate-rich foods with calcium-rich foods during meals can help reduce oxalate absorption.
4. Increase Dietary Citrate:
-Sources of Citrate:
Citrus fruits like lemons and limes are rich in citrate, which can help prevent stone formation. Regular consumption of citrus juices or adding citrus fruits to water can boost citrate levels in the urine.
-Mechanism:
Citrate binds with urinary calcium, thus reducing the supersaturation of urine and preventing the growth of crystal nuclei into larger stones.
5. Regular Monitoring:
-Urine Analysis:
Regularly testing urine output and composition is crucial for those at high risk of kidney stones. This can help track the effectiveness of dietary adjustments and hydration levels.
-Professional Guidance:
Regular check-ups with a healthcare provider can ensure that dietary and lifestyle adjustments are effectively preventing stone formation and not adversely affecting other aspects of health.
6. Additional Tips:
-Physical Activity:
Moderate, regular exercise can help manage overall body weight and can reduce the risk of kidney stone formation.
-Reduce Animal Protein:
A diet high in animal protein can increase urine acidity and reduce citrate levels, promoting stone formation. Limiting red meat, poultry, and seafood can help manage this risk.
Conclusion:
The link between salt intake and kidney stone formation is both significant and modifiable. By adopting the recommended dietary changes such as reducing sodium intake, increasing hydration, and adjusting dietary sources of calcium and oxalate individuals can greatly reduce their risk of developing kidney stones. Moreover, integrating regular health monitoring and leveraging community support can further enhance these preventive measures. Embracing these lifestyle adjustments not only contributes to kidney health but also supports overall well-being, underscoring the importance of dietary awareness in maintaining long-term health.