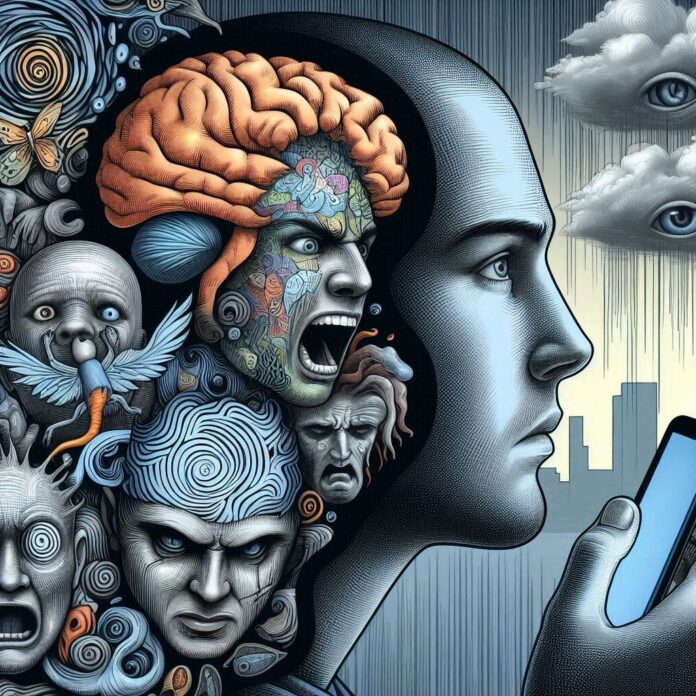
Schizophrenia is a complex and chronic mental disorder that significantly impacts an individual’s thoughts, emotions, and behaviors. Affecting approximately 1% of the global population, it manifests through a diverse range of symptoms, including hallucinations, delusions, disorganized thinking, and impaired cognitive functioning. The condition often emerges in late adolescence or early adulthood, posing considerable challenges for diagnosis and treatment. Understanding the symptoms, causes, and risk factors of schizophrenia is crucial for early detection and effective management. This comprehensive article delves into the multifaceted nature of schizophrenia, exploring its symptoms, underlying genetic and environmental causes, and the various factors that increase the risk of developing this debilitating disorder.
I. Symptoms of Schizophrenia:
Schizophrenia is a chronic mental disorder that profoundly affects how individuals think, feel, and behave. The symptoms of schizophrenia are diverse and can be categorized into positive, negative, and cognitive symptoms. Understanding these symptoms is crucial for early diagnosis and effective management of the condition.
1. Positive Symptoms:
Positive symptoms of Schizophrenia refer to those that add abnormal experiences in a person’s life. These symptoms include:
-Hallucinations:
Individuals may see, hear, feel, or even smell things that are not present. Auditory hallucinations, such as hearing voices, are the most common. These voices can comment on the person’s behavior, carry on conversations, or give commands. Visual and tactile hallucinations are also possible but less common.
-Delusions:
These are false beliefs that are not based on reality. People with schizophrenia might believe they are being persecuted, that they have extraordinary powers, or that they are someone famous. Delusions can be bizarre, such as believing that others can hear one’s thoughts, or more plausible but still unfounded.
-Disorganized Thinking and Speech:
Schizophrenia can cause significant disruptions in thought processes, leading to disorganized thinking. This manifests in a speech that is hard to follow, with individuals often jumping from one topic to another without a logical connection. They may also make up words or use words in unusual ways.
-Disorganized or Abnormal Motor Behavior:
This can range from childlike silliness to unpredictable agitation. It includes behaviors that are not goal-directed, making it hard for the person to perform daily activities.
Catatonia, where a person may become unresponsive to the environment, is a severe form of this symptom.
2. Negative Symptoms:
Negative symptoms of Schizophrenia are those that reflect a reduction or loss of normal functions. They can significantly impair an individual’s ability to function in daily life and are often more difficult to treat than positive symptoms. They include:
-Affective Flattening:
This refers to a reduced emotional expression. Individuals with affective flattening may show limited facial expressions, speak in a monotone, and exhibit a flat affect. This lack of emotional response can be misinterpreted by others as disinterest or detachment, further isolating the individual.
-Anhedonia:
This is a decreased ability to experience pleasure from once enjoyable activities. People with anhedonia may lose interest in hobbies, social interactions, and other activities that used to bring joy. This symptom can lead to a withdrawal from social life and a lack of engagement in daily activities.
-Avolition:
Avolition is a lack of motivation to initiate and sustain purposeful activities. Individuals may neglect personal hygiene, fail to complete tasks, and lack the drive to pursue goals. This can severely impact their ability to manage daily life and maintain relationships and employment.
-Alogia:
Reduced speech output is another negative symptom. This can manifest as brief, empty replies to questions and a general reduction in the fluency and productivity of speech. Alogia is often a reflection of the disorganized thinking processes that accompany schizophrenia.
-Social Withdrawal:
People with schizophrenia often isolate themselves from social interactions, have difficulty maintaining relationships, and prefer to be alone. This withdrawal can be due to a combination of other negative symptoms, such as anhedonia and avolition, and can lead to further social and functional decline.
3. Cognitive Symptoms:
Cognitive symptoms of Schizophrenia involve difficulties with mental processes and can significantly affect a person’s ability to function day-to-day. These symptoms are often subtle and may be mistaken for laziness or lack of effort.
They include:
-Poor Executive Function:
This involves difficulty in understanding information and using it to make decisions. Individuals with poor executive function may struggle with problem-solving, planning, and organizing their thoughts and activities. This can make tasks that require complex thinking or multi-step processes particularly challenging.
-Trouble Focusing or Paying Attention:
Individuals may have difficulty concentrating on tasks, following conversations, or sustaining attention on activities. This can affect their performance at work or school and can make it difficult to complete everyday tasks. Attention deficits can also interfere with the ability to engage in social interactions and maintain relationships.
-Memory Issues:
Memory problems in schizophrenia often involve working memory, which is the ability to use information immediately after learning it. This can affect the ability to learn new information and recall it when needed. Memory issues can also make it difficult to keep track of daily activities and responsibilities, leading to a disorganized lifestyle.
4. Understanding and Managing Schizophrenia Symptoms:
Recognizing the symptoms of schizophrenia is vital for timely diagnosis and treatment. While these symptoms can be severe and disabling, early intervention, and ongoing treatment can help manage the condition effectively. Understanding the full spectrum of symptoms, including positive symptoms (hallucinations, delusions, disorganized thinking, and behavior), negative symptoms (affective flattening, anhedonia, avolition, alogia, social withdrawal), and cognitive symptoms (poor executive function, trouble focusing, memory issues), helps in providing comprehensive care and support for individuals with schizophrenia.
II. Causes and Risk Factors of Schizophrenia:
Schizophrenia is mental health disorder with no single identified cause. Instead, it results from genetic, environmental, and neurobiological factors. Understanding these causes and risk factors can help in early detection and management of the condition.
1. Genetic Factors:
Genetics plays a significant role in the development of schizophrenia. Studies have shown that individuals with a family history of schizophrenia are at a higher risk of developing the disorder. For instance, if one identical twin is diagnosed with schizophrenia, the other twin has a 50% chance of developing it, even if they were raised separately. This suggests a strong genetic component, although it is not solely deterministic. Researchers believe that multiple genes are involved, each contributing to a small increase in risk rather than a single gene being responsible.
2. Neurodevelopmental Factors:
Differences in brain development and structure are also associated with schizophrenia. Research indicates that individuals with schizophrenia may have subtle abnormalities in brain regions such as the hippocampus and frontal lobes. These differences might be due to disruptions in brain development during fetal life or early childhood, possibly triggered by prenatal factors such as maternal malnutrition, infections, or birth complications like hypoxia (lack of oxygen during birth).
3. Neurotransmitter Imbalances:
Neurotransmitters, which are chemicals that transmit signals in the brain, play a crucial role in schizophrenia. An imbalance in neurotransmitters such as dopamine and glutamate has been linked to the symptoms of schizophrenia. Elevated dopamine levels, in particular, are associated with the positive symptoms of schizophrenia, such as hallucinations and delusions. Glutamate, another key neurotransmitter, is also implicated in the disorder, with evidence suggesting that dysfunction in glutamate signaling may contribute to cognitive and negative symptoms. Medications that adjust these neurotransmitter levels, such as antipsychotics, help manage symptoms, further supporting their role in schizophrenia.
4. Environmental Factors:
Environmental factors significantly influence the risk of developing schizophrenia. Key factors include:
– Prenatal Exposure:
Conditions during pregnancy, such as exposure to infections, malnutrition, and complications like hypoxia during birth, can disrupt fetal brain development, increasing the risk of schizophrenia later in life. Studies show that maternal infections and malnutrition are linked to higher schizophrenia rates in offspring.
– Childhood Trauma:
Experiencing physical, sexual, or emotional abuse, as well as neglect during childhood, can heighten the risk. Such traumatic experiences can lead to chronic stress, which impacts brain development and function, making individuals more susceptible to schizophrenia.
– Socioeconomic Factors:
Growing up in poverty or experiencing significant social adversity can elevate the risk of schizophrenia. Factors like living in densely populated urban areas, facing social inequality, and enduring chronic stress from socioeconomic disadvantages are all linked to a higher incidence of schizophrenia.
5. Substance Use:
The use of certain substances, particularly during adolescence, is linked to an increased risk of schizophrenia. Cannabis use has been widely studied in this context. Evidence suggests that frequent cannabis use, especially of high-potency forms, can double the risk of developing schizophrenia later in life. The risk is even more pronounced for individuals who begin using cannabis at a younger age. Studies indicate that the psychoactive component of cannabis, THC, can interfere with brain development and increase susceptibility to psychosis in genetically predisposed individuals.
Other substances such as cocaine, LSD, and amphetamines are also associated with triggering psychotic episodes. These substances can exacerbate underlying vulnerabilities and potentially lead to the onset of schizophrenia. For example, cocaine and amphetamines can increase dopamine levels in the brain, which is thought to contribute to psychotic symptoms. LSD, a hallucinogen, can induce experiences similar to those of schizophrenia, such as hallucinations and delusions, in vulnerable individuals.
6. Stress and Psychosocial Factors:
Stressful life events are significant triggers for schizophrenia in individuals who are already at risk. Events such as the loss of a loved one, job loss, divorce, or important life changes can precipitate the onset of the disorder. Chronic stress can exacerbate symptoms and contribute to relapses in those already diagnosed with schizophrenia. The body’s response to stress involves the release of cortisol, a hormone that, in high levels, can adversely affect brain areas involved in emotion and cognition, potentially triggering psychotic episodes.
Additionally, psychosocial factors like social isolation, discrimination, and socioeconomic challenges can increase stress levels, further contributing to the risk of schizophrenia. Individuals experiencing long-term social adversity or significant life stressors may develop maladaptive coping mechanisms, which can heighten their vulnerability to psychosis.
7. Epigenetics:
Epigenetics, the study of how environmental factors influence gene expression, also plays a crucial role in schizophrenia. This field explores how behaviors and environmental exposures can activate or deactivate certain genes, potentially increasing the risk of developing the disorder. Epigenetic changes can occur due to various factors, including stress, diet, exposure to toxins, and prenatal environmental influences. These changes can alter gene expression without modifying the DNA sequence, thereby affecting brain development and function.
For instance, prenatal exposure to stress or malnutrition can lead to epigenetic modifications that affect fetal brain development, increasing the risk of schizophrenia. Similarly, adverse childhood experiences such as trauma and neglect can induce epigenetic changes that contribute to the development of psychosis in later life. This helps explain why some individuals with a genetic predisposition do not develop schizophrenia, while others with similar genetic backgrounds do.
8. The Multifactorial Nature of Schizophrenia:
Schizophrenia is a multifaceted disorder influenced by a combination of genetic, neurodevelopmental, environmental, and psychosocial factors. Early recognition of these risk factors can lead to better management and treatment outcomes, improving the quality of life for those affected by the disorder.
Conclusion:
Schizophrenia is a multifaceted disorder influenced by a combination of genetic, neurodevelopmental, environmental, and psychosocial factors. Recognizing the wide spectrum of symptoms from positive and negative symptoms to cognitive impairments is vital for timely diagnosis and effective treatment. Understanding the complex interplay of these factors can lead to better management strategies and improved outcomes for individuals living with schizophrenia. By addressing the genetic predispositions, environmental triggers, and the role of neurotransmitters, we can develop more targeted and effective interventions. Ultimately, increasing awareness and knowledge about schizophrenia can help reduce stigma, support early intervention, and enhance the quality of life for those affected by this challenging condition.