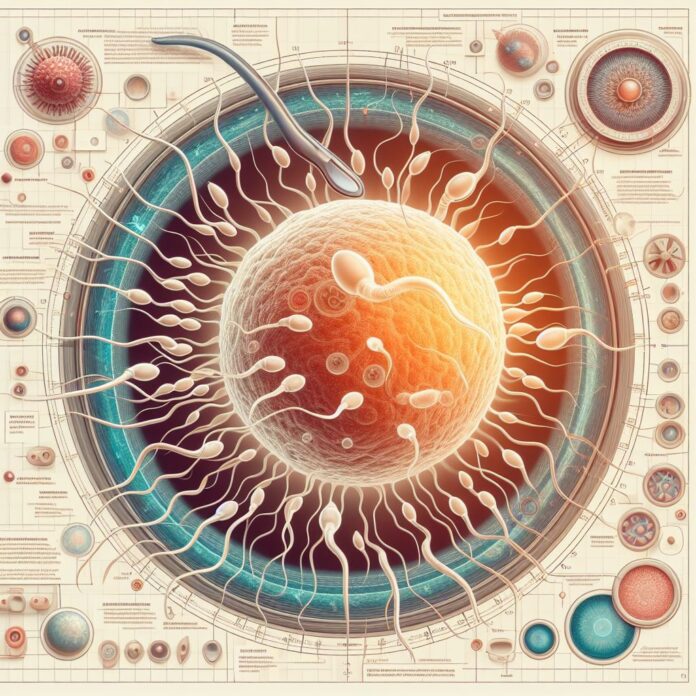
The miraculous journey of life begins with the smallest of cells sperm. These microscopic swimmers play a crucial role in human reproduction, carrying the genetic blueprint for the next generation. The production of sperm, a process known as spermatogenesis, is a complex and finely tuned operation that takes place within the male reproductive system. This system is composed of several key organs, including the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and urethra, each playing a vital role in the creation, maturation, and delivery of sperm. In this article, we will delve into the fascinating world of sperm production, exploring the anatomy of the male reproductive system, the stages of spermatogenesis, and the factors that can influence sperm health. Whether you’re seeking to understand your own body better or looking to optimize your reproductive health, this guide will provide valuable insights into the wonders of sperm production.
I. Anatomy of the Male Reproductive System:
The male reproductive system is a marvel of nature, meticulously designed to produce, store, and deliver sperm. At the heart of this system are the testes, two oval-shaped organs housed within the scrotum. The testes function as factories for sperm production, generating millions of sperm cells daily through a process called spermatogenesis. Each testis comprises tightly coiled tubes called seminiferous tubules, where sperm cells originate and commence their journey to maturity.
1. The Testes: The Heart of Sperm Production.
The testes are the primary organs of the male reproductive system, located within the scrotum. They are responsible for producing millions of sperm cells every day through a process called spermatogenesis. Inside each testis, there are seminiferous tubules where sperm cells originate and start maturing.
2. The Epididymis: Maturation Ground for Sperm.
Next to the testes is the epididymis, a long, coiled tube where sperm continue to mature. Here, they gain the ability to swim and fertilize an egg. Mature sperm are stored in the epididymis until they are ready for ejaculation.
3. The Vas Deferens: Sperm Transportation Highway.
The vas deferens is a muscular tube that carries mature sperm from the epididymis to the ejaculatory ducts during ejaculation. It’s a crucial part of the sperm’s journey, ensuring they are mixed with seminal fluid produced by the seminal vesicles, which provides nourishment and a medium for swimming.
4. The Prostate Gland: Enhancing Sperm Viability.
Located just below the bladder, the prostate gland contributes additional secretions to the seminal fluid. Its alkaline fluid enhances sperm motility and longevity and helps neutralize the acidic environment of the vagina, making it easier for sperm to survive the journey to fertilize an egg.
5. The Urethra: Final Pathway for Sperm Delivery.
The urethra is the tube that runs through the penis, serving as the final pathway for semen, which is a mixture of sperm and seminal fluid, to exit the body during ejaculation. It plays a vital role in delivering sperm to the outside world, where they can embark on their mission to fertilize an egg.
Each part of the male reproductive system plays a specific and crucial role in the production, maturation, and delivery of sperm. Understanding the anatomy of this system is essential for comprehending how sperm are produced and the factors that can influence male fertility.
II. The Spermatogenesis Process:
Spermatogenesis is a complex and fascinating process that occurs within the male reproductive system. It’s the journey that transforms immature germ cells into fully mature and motile sperm, capable of fertilizing an egg. This process is vital for reproduction and involves several stages, each orchestrated by a symphony of hormones.
1. Understanding the Stages of Spermatogenesis:
Spermatogenesis begins in the seminiferous tubules of the testes, where the foundational cells, called spermatogonia, reside. These cells divide and differentiate through several stages:
-Spermatogonia: These are the starting cells, which undergo mitotic division to either maintain their population or differentiate into the next stage.
-Primary Spermatocytes: After differentiation, spermatogonia become primary spermatocytes, which are larger cells that undergo the first meiotic division.
-Secondary Spermatocytes: The primary spermatocytes divide to form secondary spermatocytes, which then undergo the second meiotic division.
-Spermatids: The result of the second meiotic division, spermatids are haploid cells that begin the process of spermiogenesis.
-Mature Sperm: Through spermiogenesis, spermatids undergo physical transformation to become mature sperm, developing tails for motility and condensing their nuclei for efficient DNA delivery.
2. The Role of Hormones in Regulating Spermatogenesis:
Hormones play a crucial role in regulating spermatogenesis, ensuring that sperm are produced at the right time and in the right quantities:
– Follicle-Stimulating Hormone (FSH): Secreted by the pituitary gland, FSH stimulates the Sertoli cells in the testes, which are essential for nurturing the developing sperm cells.
– Luteinizing Hormone (LH): Also produced by the pituitary gland, LH triggers the Leydig cells in the testes to produce testosterone, a hormone crucial for the final stages of sperm maturation.
– Testosterone: This hormone is essential for the development and maintenance of male reproductive tissues and plays a direct role in the maturation of sperm.
Spermatogenesis is a highly orchestrated process that ensures the continuous production of healthy and motile sperm. Understanding this process and the hormonal regulation involved is crucial for anyone interested in reproductive biology or seeking to address issues related to male fertility.
III. Maturation and Storage of Sperm:
The journey of sperm from production to ejaculation is a complex and finely tuned process. After forming in the testes, sperm undergo crucial maturation and storage phases that prepare them for their ultimate mission: fertilization. These final stages take place in specialized structures within the male reproductive system, ensuring that sperm are fully equipped for their journey ahead.
1. The Epididymis: A Crucible of Maturation.
The epididymis, a long, coiled tube attached to the back of each testis, serves as the primary site for sperm maturation. Freshly produced sperm are immature and cannot swim or fertilize an egg. As they travel through the epididymis, they undergo a series of transformations. Key changes include the acquisition of motility, which enables them to swim towards the egg, and the maturation of their membrane, which is essential for successful egg penetration. This process typically takes about two to three weeks, after which the sperm are considered mature and capable of fertilization.
2. Storage and Nutritional Support: Seminal Vesicles and Prostate Gland.
Once mature, sperm are stored in the tail of the epididymis, awaiting the signal for ejaculation. However, sperm alone does not make up the semen that is ejaculated. Semen is a mixture of sperm and fluids from various glands, each contributing to the overall composition and function of the ejaculate.
The seminal vesicles, two small glands located near the base of the bladder, produce a viscous fluid rich in fructose. This fluid provides a source of energy for the sperm, fueling their journey through the female reproductive tract. The fluid from the seminal vesicles also contains substances that help in the coagulation and subsequent liquefaction of semen, which are important for sperm release and mobility post-ejaculation.
The prostate gland, situated just below the bladder, adds a thin, alkaline fluid to the semen. This fluid plays multiple roles: it helps neutralize the acidic environment of the vagina, increasing the lifespan of sperm; it contributes to sperm motility; and it contains enzymes that aid in semen liquefaction, which is crucial for freeing the sperm to swim towards the egg.
The maturation and storage of sperm in the epididymis, along with the nourishment and support provided by the seminal vesicles and prostate gland, are essential components of the male reproductive system. These processes ensure that sperm are ready and capable of embarking on their vital mission of fertilization when the moment arrives.
IV. Factors Affecting Sperm Production:
In the intricate dance of human reproduction, sperm production plays a pivotal role. The journey from a single cell to a fully formed spermatozoon is a complex process, influenced by a myriad of factors. Understanding these factors is crucial, not only for those navigating the challenges of fertility but also for anyone interested in maintaining optimal reproductive health. We’ll explore the various lifestyle, environmental, and medical elements that can impact sperm production and quality.
1. Lifestyle Choices: The Cornerstone of Sperm Health.
-Diet: A balanced diet rich in antioxidants, vitamins, and minerals is essential for optimal sperm production. Foods high in zinc, such as oysters, pumpkin seeds, and nuts, can enhance testosterone levels and sperm count. Omega-3 fatty acids, found in fish like salmon, also play a crucial role in sperm membrane development.
-Exercise: Regular physical activity can boost testosterone levels, improve sperm quality, and increase libido. However, excessive exercise or activities that raise scrotal temperature, like cycling, can have adverse effects.
-Smoking: Tobacco smoke is laden with harmful chemicals that can damage sperm DNA, reduce sperm count, and impair fertility. Quitting smoking can significantly improve sperm quality.
-Alcohol: Moderate alcohol consumption may not have a significant impact, but excessive drinking can reduce testosterone levels, decrease sperm production, and lead to erectile dysfunction.
2. Environmental Influences: Navigating the Invisible Threats.
-Temperature: The testicles are housed outside the body for a reason – to keep them cooler than the rest of the body. Elevated temperatures from hot baths, saunas, or tight clothing can impair sperm production.
-Toxins: Exposure to environmental toxins like pesticides, heavy metals, and industrial chemicals can have detrimental effects on sperm count and quality. Minimizing exposure and using protective gear when necessary is advisable.
3. Medical Conditions: The Silent Saboteurs.
-Varicocele: This condition involves the enlargement of veins within the scrotum, leading to increased temperature and reduced sperm quality. Treatment options include surgery or embolization to alleviate the issue.
-Hormonal Imbalances: Testosterone and other hormones play a crucial role in sperm production. Disorders such as hypogonadism (low testosterone) can lead to reduced sperm count and infertility.
Sperm production is influenced by a delicate balance of lifestyle choices, environmental exposures, and underlying medical conditions. By understanding and addressing these factors, individuals can take proactive steps to enhance their reproductive health and fertility. Whether it’s through dietary adjustments, lifestyle modifications, or seeking medical intervention for underlying conditions, the path to improved sperm production is within reach.
V. Improving Sperm Production and Health:
In the journey towards building a family, the health of sperm plays a crucial role. With concerns about declining sperm counts globally, it’s more important than ever to focus on factors that can enhance sperm production and overall health. We’ll explore practical tips for maintaining a healthy lifestyle and the significance of regular medical check-ups in safeguarding fertility.
1. Embracing a Healthy Lifestyle: The Foundation of Sperm Health.
-Nutritious Diet: A diet rich in antioxidants, vitamins, and minerals are essential for optimal sperm health. Incorporate foods high in zinc, selenium, and folic acid, such as lean meats, nuts, and leafy greens. Omega-3 fatty acids, found in fish like salmon and walnuts, are also beneficial for improving sperm quality.
-Regular Exercise: Engaging in moderate physical activity can boost testosterone levels and improve sperm concentration and motility. Aim for at least 30 minutes of exercise most days of the week, but avoid activities that could increase scrotal temperature, such as long-distance cycling.
-Maintain a Healthy Weight: Obesity can negatively impact sperm count and quality. Achieving and maintaining a healthy weight through diet and exercise can enhance fertility.
-Avoid Harmful Substances: Smoking, excessive alcohol consumption, and recreational drug use can significantly reduce sperm production and quality. Limiting alcohol intake and avoiding tobacco and illicit substances are crucial steps for improving sperm health.
-Manage Stress: Chronic stress can interfere with hormonal balance and sperm production. Incorporate stress-reduction techniques such as meditation, yoga, or deep breathing exercises into your daily routine.
-Stay Hydrated: Adequate hydration is vital for all bodily functions, including sperm production. Aim to drink at least eight glasses of water a day.
2. The Role of Regular Medical Check-Ups:
-Early Detection: Regular visits to a healthcare provider can help identify and address any underlying medical conditions that may affect fertility, such as varicocele, infections, or hormonal imbalances.
-Personalized Advice: A healthcare professional can offer tailored advice based on your specific health needs and fertility goals, including guidance on supplements or medications that may improve sperm health.
-Monitoring Progress: Regular check-ups allow for monitoring the effectiveness of lifestyle changes and treatments, enabling adjustments as needed to optimize results.
Improving sperm production and health is a multifaceted approach that involves maintaining a healthy lifestyle and seeking regular medical care. By adopting these strategies, individuals can enhance their fertility prospects and take proactive steps toward achieving their family-building goals.
In the pursuit of enhancing sperm production and quality, some men turn to dietary supplements like Semenax. Semenax is a supplement designed to increase sperm volume, improve sperm motility, and enhance the intensity of orgasms. It contains a blend of natural ingredients such as plant extracts, amino acids, and minerals, which are believed to support the overall health of the male reproductive system. Before adding Semenax or any other supplement to your routine, it’s important to consult with a healthcare professional to ensure it’s safe and suitable for your individual needs.
Conclusion:
The journey of sperm production is a remarkable testament to the intricacies of the human body. Understanding the anatomy of the male reproductive system, the stages of spermatogenesis, and the factors that influence sperm health is essential for anyone looking to optimize their fertility or simply gain insight into this fascinating biological process. By adopting healthy lifestyle choices, being mindful of environmental factors, and seeking regular medical check-ups, individuals can take proactive steps to enhance their sperm production and overall reproductive health. As we continue to unravel the mysteries of sperm biology, it’s clear that these tiny cells play a monumental role in the miracle of life, underscoring the importance of nurturing and protecting our reproductive well-being.